The Department of Technology Partners (DTP) at Mount Sinai hosts a Big Data and AI Forum periodically. The latest event took place on May 9th, 2023 and covered a host of new machine learning projects, including:
- Hospital Acquired Pressure Injury Risk Predictions (HAPI)
- 48Hrs Discharge Planning Tool 2.0
- HeartBEit: Integrating ECGs as language
- BMEII AI Core
Below are some of the highlights from the Clinical Data Science team:
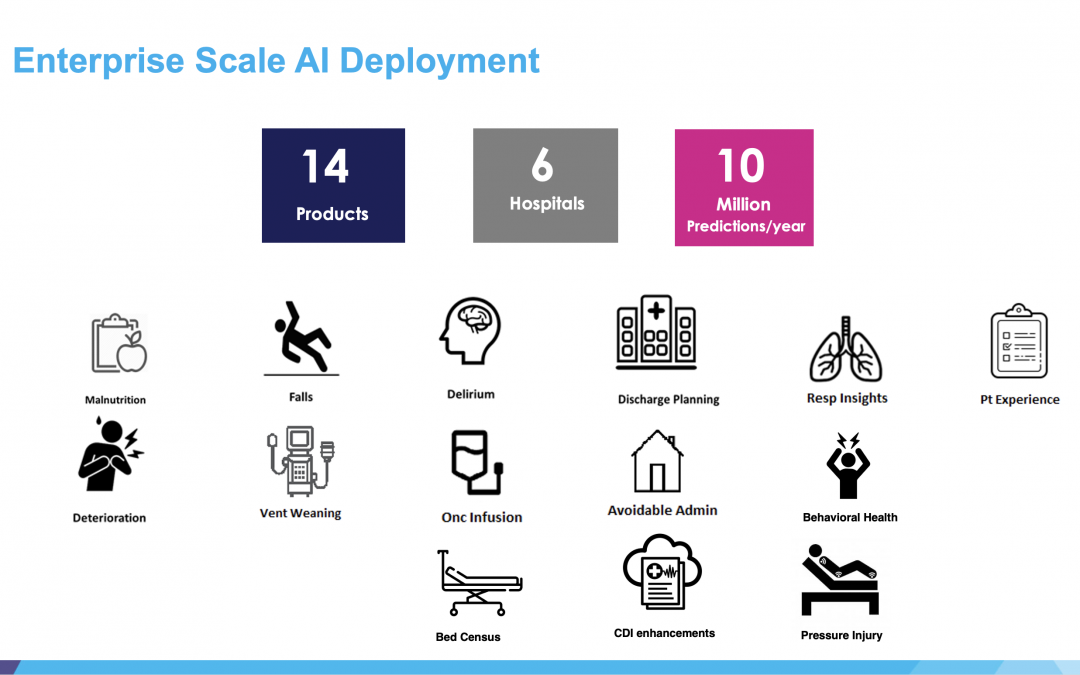
The Clinical Data Science team has deployed 14 applications throughout six hospital in the Mount Sinai Hospital System. These applications make over 10 million predictions a year in areas such as:
- Malnutrition
- Fall Prevention
- Delirium Detection
- Discharge Planning
- Respiratory Insights
- Patient Experience
- Patient Health Deterioration
- Vent Weaning
- Oncology Infusion
- Avoidable Admissions
- Behavioral Health
- Bed Census
- Pressure Injury
The team presented new projects in two of these areas: pressure injury and discharge planning:
Project 1 – Hospital Acquired Pressure Injury Risk Prediction (HAPI)
Presented by Nhi Nguyen, M. Sc.
HAPI: definition
- Pressure injury/ulcer: localized injury to the skin and/or underlying tissue, result from compression between a bony prominence and an external surface for a prolonged time
- HAPI (hospital-acquired pressure injury): during an inpatient hospital stay
- CAPI (community-acquired pressure injury): acquired outside the hospital
Challenges
- Increased length of stay by 3-7 days [1]
- Not reimbursed by CMS
- Costly: $12K-40K per pressure injury [2]
Opportunities
- Identify patients at highest risk of developing HAPI with a predictive machine learning model
- Take preventative measures with WOCNs (Wound Care Nurses) to prevent HAPIs
Benchmark: the Braden Scale
- Tool to assess and document patient’s risk for developing HAPIs (done at every shift for every patient)
- Risk factors are rated on a scale from 1 to 4 and added
- The total score indicates a patient’s risk for developing a HAPI
Historical Cohort
Inclusion Criteria:
Age >= 18
Facility: MSH
Referred for a WOCN consult
Exclusion Criteria:
Patients with CAPIs (community-acquired pressure injury)
LOS < 2 days and > 180 days
Data:
WOCN consult notes
ADT
Vitals, Labs, Nursing Flowsheets
Source: Epic, CERNER, Clarity
Data Timeframe: March 2018 to January 2023
Cohort Characteristic and Labeling Logic
Both data logics were validated via extensive chart reviews with WOCN from MSH, MSB and MSW
Gave ~98% accuracy
| HAPI label | Definition | Label timestamp |
| 1 | Hospital-acquired pressure injury only | First HAPI |
| 0 | No pressure injury during the visit | Discharge date |
Modeling and Results
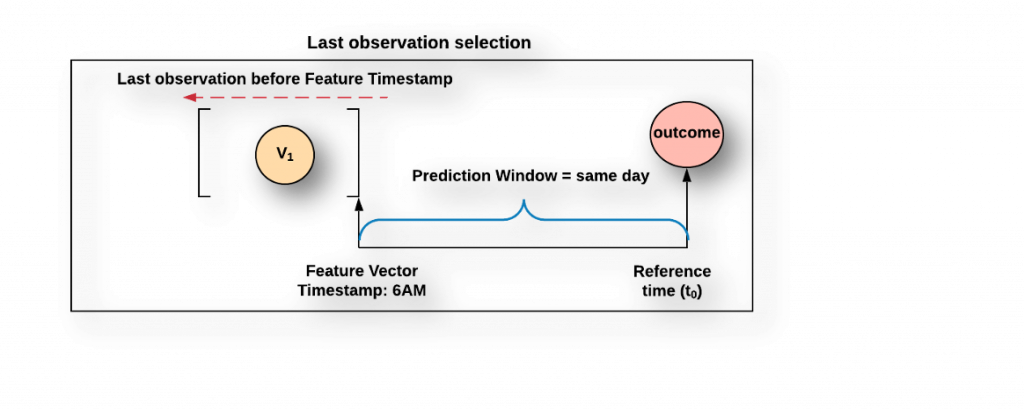
Sampling Logic
Last observation selection:
For less frequent variables (e.g.: weight, blood culture)
Regular sampling:
For frequently available variables (e.g.: O2 saturation, respiration)
Best Model: XGBoost classifier
| Data set | Time Frame | # visits | # HAPIs (%) | Threshold | Sensitivity | Specificity | Precision | Accuracy | F1-Score | AUC |
| Test | 01/01/2018 – 01/15/2023 | 1776 | 314 (18%) | 0.48 | 0.76 | 0.74 | 0.39 | 0.74 | 0.51 | 0.83 |
| Hold-Out (MSH) | 01/01/2016 – 12/31/2017 & 01/16/2023 – 02/12/2023 | 1820 | 197 (11%) | 0.48 | 0.74 | 0.76 | 0.27 | 0.76 | 0.40 | 0.83 |
| Hold-Out (non-MSH) | 07/13/2021 – 03/17/2023 | 3831 | 204 (5%) | 0.3 | 0.70 | 0.75 | 0.14 | 0.74 | 0.23 | 0.81 |
Next Steps
- Deploy the application for Mount Sinai Hospital
- Start the silent pilot and identify the best threshold for the active pilot units
- Identify the acceptance criteria for scaling up across MSH units
- Scale across MSH
- Develop a scaling plan for and scale across MSB, MSW, MSM, MSQ, MSBI
Project 2 – 48Hrs Discharge Planning Tool V2.0: Optimizing Discharge Process Through Hybrid NLP-EMR Approach
Optimization Opportunity and Main Goal
Challenges
- Multidisciplinary Decision Making
- Fragmented Teams
- Prolonged LOS
- Patient Safety: HAI, and Risk of Adverse Events
- Patient Satisfaction
- Resource Management : Service Quality
- Resource Utilization and Cost of care
Opportunity: Optimize discharge process by identifying clinically ready patients 48hrs in advance
Goal: Develop a classifier to predict likelihood of clinically readiness within 48 hrs.
Historical Cohort Characteristics
Facility: MSH
Data: ADT, Vitals, Labs, Nursing flowsheets, Progress Notes, Care Notes
Inclusion Criteria: Age>=18, Patient Class: Inpatient, LOS>=48 hrs
Exclusion Criteria: PoC = ICU, Death Flag = Y
Source: CERNER, SCC, EPIC
Date of Case Manager Flowsheet: July 2019 to January 2022
Labeling and Sampling Logic
|
Label definition |
Label Timestamp |
Reference Timestamp |
|
|
Positive |
•”Clinically ready = Y” •”Clinically ready = N” AND “Discharge – Prediction < 3 days”
|
CM flowsheet timestamp |
CM flowsheet Date |
|
Negative |
“Clinically ready = N” AND “Discharge – Prediction >= 3days” |
CM flowsheet timestamp |
CM flowsheet Date |
Historical Model Performance
Random Forest default threshold = 0.50
|
Dataset |
Sample Size |
Positive Rate (%) |
Sensitivity (%) |
Specificity (%) |
Precision (%) |
Accuracy (%) |
AUC |
|
Train |
9381 |
50 |
99.2 |
95.2 |
95.4 |
97.2 |
99.4 |
|
Test |
5557 |
62 |
66.2 |
68.2 |
75.4 |
63.6 |
70.2
|
Top 20 Predictors
|
Top 20 most important variables |
|||
|
1 |
Temperature (Oral) |
11 |
Potassium |
|
2 |
Diastolic BP |
12 |
Glucose |
|
3 |
Systolic BP |
13 |
BUN |
|
4 |
Albumin |
14 |
Hgb |
|
5 |
O2 Saturation |
15 |
Platelet |
|
6 |
Chloride |
16 |
INR |
|
7 |
Hospital SVC |
17 |
Creatinine |
|
8 |
Sodium |
18 |
Age |
|
9 |
WBC |
19 |
Respiratory Pattern |
|
10 |
Calcium |
20 |
Admit Source |
Hold-out Set Performance
Random Forest based on balanced threshold
|
Dataset |
Sample Size |
Positive Rate (%) |
Threshold |
Sensitivity (%) |
Specificity (%) |
Precision (%) |
Accuracy (%) |
AUC |
|
V1.0 |
7074 |
79 |
0.64 |
57 |
55 |
83 |
56 |
0.59 |
|
V2.0 |
7074 |
79 |
0.51 |
61 |
63 |
86 |
61 |
0.67 |
Next Steps
- Deploy in QA and measure the silent pilot performance
- Develop upgrade plan for MSH
- Upgrade the current engine to V2.0 in MSH