The 48Hr Discharge (aka Length of Stay) streaming engine was created to predict the probability of patient discharge (by 2pm and midnight daily) and therefore help automate the RTDC system and assist in the prioritization of remaining tasks at Mount Sinai Hospital. This model was deployed at Mount Sinai Hospital in July of 2019 and uses a random forest classifier.
Rationale
- Optimal patient flow facilitates beneficial treatment, minimal waiting, minimal exposure to risks associated with hospitalization, and efficient use of resources (e.g., of beds, clinical staff, and medical equipment)[1]
- For patients, prolonged hospital stays increase the risk of adverse events, such as hospital-acquired infections, adverse drug events, poor nutritional levels, and other complications[1]
- Extended stays have also been associated with poor patient satisfaction[1]
- Healthcare costs as a percentage of GDP (17.9% in 2012) have been rising faster than anticipated,18 and approximately 30–40% of these expenditures have been attributed to overuse, underuse, misuse, duplication, system failures, unnecessary repetition, poor communication, and inefficiency.[1]
- sociodemographic and disease-specific factors associated with PLOS [3]
- Another solution to the above: predicting patient readmission
Definitions
Patient Flow
- We can view flow from two perspectives, the operational and the clinical [2]
- Operational – the movement of patients through a set of locations in a health care facility
- Models provide very accurate predictions yet are very costly and time consuming to build [2]
- Models not easily generalized
- Clinical – the progression of a patient’s health status
- less costly and time consuming than the operational models
- Operational – the movement of patients through a set of locations in a health care facility
Length of Stay (LoS)
- The duration of a single episode of hospitalization (measured in days)
- Has been employed as a proxy for measuring the consumption of hospital resources
Excess Days
- The number of days a patient stays in the hospital greater than the expected normal LoS
- Optimization of patient flow process results in fewer excess days
PLOS vs NLOS
acc. to source [3]
- Normal LoS (NLOS) — LoS < 34 days
- Prolonged LoS (PLOS) — LoS >= 34 days (not necessarily as a result of excess days)
Process Flow
- Clinical
- Operational
Conventional tools
- Real-time demand capacity management (RTDC) – a system where clinicians meet each morning to predict patients able to leave the same day and prioritize their remaining tasks for early discharge (not automated) [1]
- Tool 1 – supervised machine learning model
- Goal – a model to predict probability of patient discharge (by 2pm and midnight daily) to automate the RTDC system and assist in the prioritization of remaining tasks [1]
- Method
- logistic regression as baseline for comparison
- applied tree-based supervised machine learning methods for predictions
- regression random forest (RRF) proved most accurate
- Performance
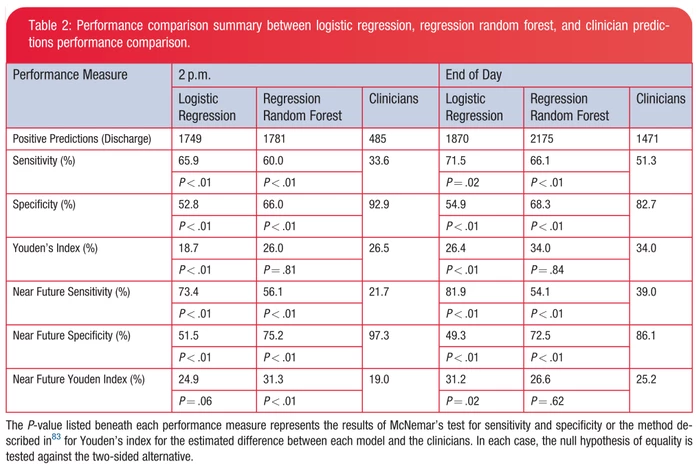
- the model outperformed the clinicians for some near-future (meaning the prediction was correct within a day) and aggregate prediction metrics\
- Impact
- there is high potential for these models to automate and expedite the RTDC prediction process
- models were applied to simple and readily accessible information that can be powerful, and easily replicated
- Tool 2 – Elderly Patient LoS Predictor[4]
- Goal
- Introduce new methodology of modelling patient pathways
- Accurate prediction of elderly patient LoS
- Method
- Uses phase-type survival tree to cluster patients into different cohorts based on their covariates and length of stay in hospital
- Partitions the movement of patient cohorts into multiple ordered stages: initial hospital admission, first community stage, first hospital readmission stage, second community stage, and second hospital readmission stage
- Different cohorts have different discharge and death distributions
- make separate predictions for different cohorts
- Coxian phase-type distribution to model the pathway for each cohort, calculating conditional probability for length of stay at the current stage of care
- Uses phase-type survival tree to cluster patients into different cohorts based on their covariates and length of stay in hospital
- Performance
- the survival tree methodology of dividing patients into cohorts was successful
- 53 LoS median values out of the 56 distributions (different stages of care for each cohort) fell within the empirical 95% confidence interval (CI)
- the remaining 3 cases failed only due to lack of data
- 53 LoS median values out of the 56 distributions (different stages of care for each cohort) fell within the empirical 95% confidence interval (CI)
- the survival tree methodology of dividing patients into cohorts was successful
- Impact
- has the potential to become a decision support tool to predict:
- when a given patient is likely to leave hospital upon entering the department
- when they are likely to be readmitted to hospital upon their discharge to the community
- has the potential to become a decision support tool to predict:
- Important Notes
- reason for admission was intentionally omitted from the study (though it does play a large role in LoS)
- related hospital admissions which took place prior to the study were excluded
- type of community care was not specified (eg. residential care or patients own home)
- Goal
- Tool 3 – Penn hospital LoS Predictor
- Goal
- compare performances of three different ML models to predict LoS in all federal and specialty hospitals in Pennsylvania
- Method
- ANCOVA indicates Admission and Beds Staffed play a major role in predicting LOS
-
- Classification and regression tree (CART)
- Chi-squared automatic interaction detection (CHAID)
- Support vector regression (SVR)
- ensemble prediction using average of all three methods
- Uses v-fold validation to validate the model and compare predictive performance
- Goal
- In one study (not a developed tool) [2]
- probabilistic solutions for modelling LoS
- Markov models
- phase-type distributions
- conditional phase-type distributions
- modelling
- Mixed Exponential Distributions
- Compartmental modelling
- Simulation modelling
- probabilistic solutions for modelling LoS
- Tool 1 – supervised machine learning model
References
- Barnes, S., Hamrock, E., Toerper, M., Siddiqui, S., & Levin, S. (2016). Real-time prediction of inpatient length of stay for discharge prioritization. Journal of the American Medical Informatics Association, 23(e1), e2–e10. https://doi.org/10.1093/jamia/ocv106
- A., M., C., V., & E., E.-D. (2005). Length of stay-based patient flow models: Recent developments and future directions. Health Care Management Science, 8(3), 213–220. https://doi.org/10.1007/s10729-005-2012-z
- Marfil-garza, B. A., Belaunzarán-zamudio, P. F., Gulias-herrero, A., Kershenobich-stalnikowitz, D., & Sifuentes-osornio, J. (2018). PLOS ONE Full Risk factors associated with prolonged hospital length-of-stay : 18-year retrospective study of hospitalizations in a tertiary healthcare center in Mexico, 4–17. https://doi.org/10.1371/journal.pone.0207203
- Gordon, A. S., Marshall, A. H., & Zenga, M. (2018). Predicting elderly patient length of stay in hospital and community care using a series of conditional Coxian phase-type distributions, further conditioned on a survival tree. Health Care Management Science, 21(2), 269–280. https://doi.org/10.1007/s10729-017-9411-9
- Pendharkar, P. C., & Khurana, H. (2014). Machine learning techniques for predicting hospital length of stay in pennsylvania federal and specialty hospitals. International Journal of Computer Science and Applications, 11(3), 45–56.
- Morton, A., Marzban, E., Giannoulis, G., Patel, A., Aparasu, R., & Kakadiaris, I. A. (2014). A comparison of supervised machine learning techniques for predicting short-term in-hospital length of stay among diabetic patients. Proceedings – 2014 13th International Conference on Machine Learning and Applications, ICMLA 2014, 428–431. https://doi.org/10.1109/ICMLA.2014.76

